Induction Chemotherapy — Introduction
Induction chemotherapy, for AML, typically involves something called “7+3” which refers to 7 days of continuous cytarabine in addition to 3 days of either idarubicin or daunorubicin.
Because of the leukemic blast cells in the body, “7+3” was started for my dad. He had a PICC line placed, which is a sort of large IV that is semi-permanent and is able to deliver the toxic chemo, and then started on the chemotherapy.
Here you can see how Dad’s WBC (white count) dropped quickly once chemo was started (HOD refers to HOspital Day). This was done initially with hydroxyurea (HOD 1 and 2) and then with Idarubicin (HOD 3-5) and Cytarabine (HOD 3-10). It wasn’t until day 25 or so when his WBC started to rise again after being wiped out. In the interim, he dealt with mouth ulcers, gum and tooth pain, sequelae from low platelets, leg and ankle edema and swelling, and fatigue, among other things.
This graph shows the highest temperature Dad had each day of the hospital. The fevers that he had when he first arrived at the hospital ended on day 3 (days 3 through 8 temperatures were poorly recorded but he had no fevers during this time, hence the normal of 98.6).. He had 2 fevers during his stay, both of which were when he was very neutropenic and both of which were treated with IV antibiotics. We believe the infection may have either been from his gut or his gums. His temperature normalized after the second episode.
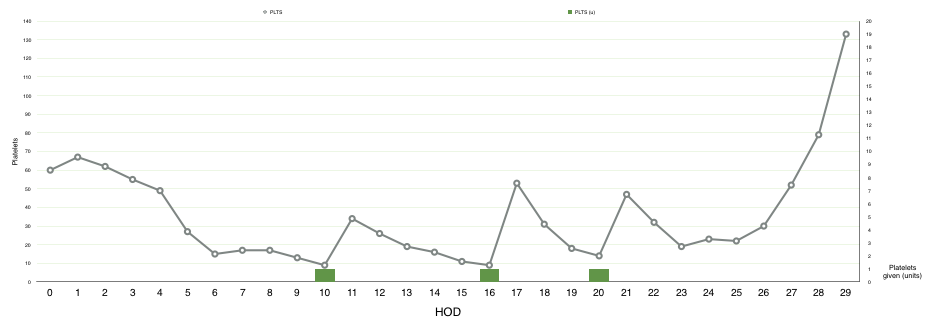
His hemoglobin went down and he needed blood transfusions. His platelets went down and he needed platelet transfusions.
This shows Dad’s hemoglobin throughout his induction chemotherapy. It was already low, around 10, when he was first admitted because the leukemia in his bone marrow was making it difficult to produce more blood. With chemotherapy, the hemoglobin and red blood cells trended down, requiring blood transfusions (on HOD 8, 17, and 21) to keep his count about 7. Transfusions become more frequent as time goes on but thankfully his bone marrow recovered towards the end of his hospital stay and was able to make enough red blood cells that it was able to increase without the use of platelets.
Similarly, Dad’s platelets fell because of the chemotherapy and required 3 platelet transfusions after which on day 23 his counts started to recover dramatically. Platelets are typically given 1 unit at a time as opposed to the pRBC (packed red blood cells for hemoglobin) which are given 2 units at a time.
After the 7+3 component of his treatment, we found that he had the FLT3 mutation, in addition to NPM1 and DNMT3A. Because of the FLT3, he was started on 2 weeks of midostaurin (Rydapt) afterwards.
This shows how Dad’s hemoglobin and ANC (one of the components of the white count) correlated with his overall state, a subjective grading from 1 to 10 on his overall functional status and well being that I gave every day, his appetite (subjectively graded from 1 to 5), and the number of miles he walked in the hallways. Overall, his overall state, appetite, and number of miles walked per day improved through the course of his hospital day. However, acute decreases in those things correlated well with his drops in hemoglobin and improved after transfusion. Once his ANC started coming up, he started to feel much better.
Overall, things got better with time. His blood counts started to creep up during week 4 and he was deemed safe for discharge during week 5 after a repeat bone marrow biopsy showing a hypocellular marrow with no evidence of blasts…remission.